Between 10-20% of children globally have Atopic Dermatitis, a chronic but non-contagious skin disease that also affects adults. Also known as Atopic Eczema, typical symptoms include dry, irritable skin which occasionally flares-up causing mild to intense itching, inflammation and soreness. While there is no known cure, regular and consistent care can help to alleviate the symptoms and prolong the non flare-up phases.
Signs & Symptoms
What is Atopic Dermatitis?
Atopic Dermatitis (or Atopic Eczema) is an uncomfortable and sometimes distressing long-lasting skin disease that is very common in children across the globe, although predominantly in the Western world. While around 2-5% of adults are affected, 10-20% of patients are children and babies. Most sufferers (90%) get Atopic Dermatitis before the age of five and many children do grow out of the disease.
Typically Atopic Dermatitis goes through two “phases”. During an inactive phase skin is very dry, irritable and flaky and needs to be moisturised on a daily basis. Active phases (or “flare-ups”) are more painful and need to be treated with topical medications to calm inflamed skin and alleviate itching.
Atopic Dermatitis looks and feels different in babies, children and adults:
- Babies can develop symptoms as young as 2-3 months. A rash may appear suddenly which makes skin dry, scaly itchy. In flare-up phases, infected skin may ooze fluid.
- When children develop the disease later in life (between the ages of two and puberty) the rash is usually dry with itchy, scaly patches. Skin tends to be bumpy, thickened and leathery.
- Adult Atopic Dermatitis, which usually begins in childhood, is typified by very dry, scaly skin and a non-stop itch.


The most common areas for Atopic Dermatitis to appear on babies is the face and scalp (especially on the cheeks) as well as the body (elbows and knees).
With children that develop the disease after babyhood, the rash often begins on the body - in the creases of the elbows or knees - and it is common to see a young patient with atopic skin on his or her neck, wrists, ankles and/or the creases between the buttocks and legs.
Atopic Dermatitis is made worse by scratching as nails break through the skin barrier and expose bacteria, causing skin to get inflamed. Babies often rub their skin against bedding or carpeting to relieve the itch and in children of all ages, the itch can become so intense that they cannot sleep. As well as being distressing for the child, parents can feel powerless to help which, in turn causes psychological stress. The good news is that effective treatment and good skin care can alleviate much of the discomfort.
Attention
If you are unsure about your symptoms seek the advice of a doctor or dermatologist.
Read more about children’s skin.
Causes & Triggers
Potential causes and triggers of Atopic Dermatitis
Dermatologists have identified several causative and contributory factors. For example:


- Family members have Atopic Dermatitis, hay fever and/or asthma. There is a known link between Atopic Dermatitis, hay fever and asthma and evidence shows that if one or both parents suffer from any, or all, of these conditions, their children will be more at risk.
- The child lives in a developed country, possibly a city, where pollutants are higher or he or she lives in a cold climate. Interestingly, Jamaican children living in London are twice as likely to develop Atopic Dermatitis as those that live in Jamaica.
- She’s a girl. Females are slightly more likely to get the disease than males.
- Her mother gave birth later in life. There is evidence to show that babies born in the later stages of a mother’s child-bearing years have a higher propensity to Atopic Dermatitis.
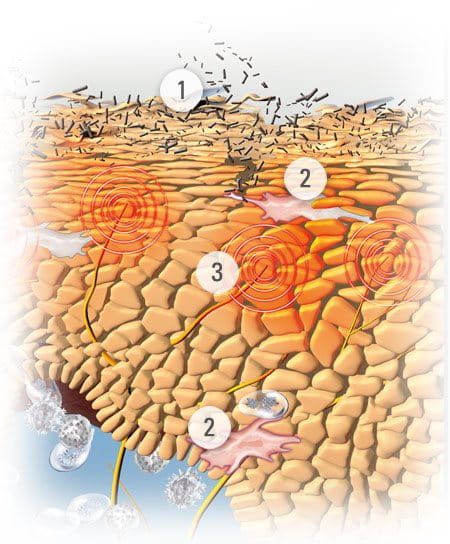
Once affected, there are a number of reasons why symptoms get worse or flare-ups occur. Sufferers have a deficiency of natural moisturising factors (NMFs) (such as amino acids) and disturbance of the epidermal lipid metabolism. This explains why their skin is more likely to be dry with a disturbed barrier function.
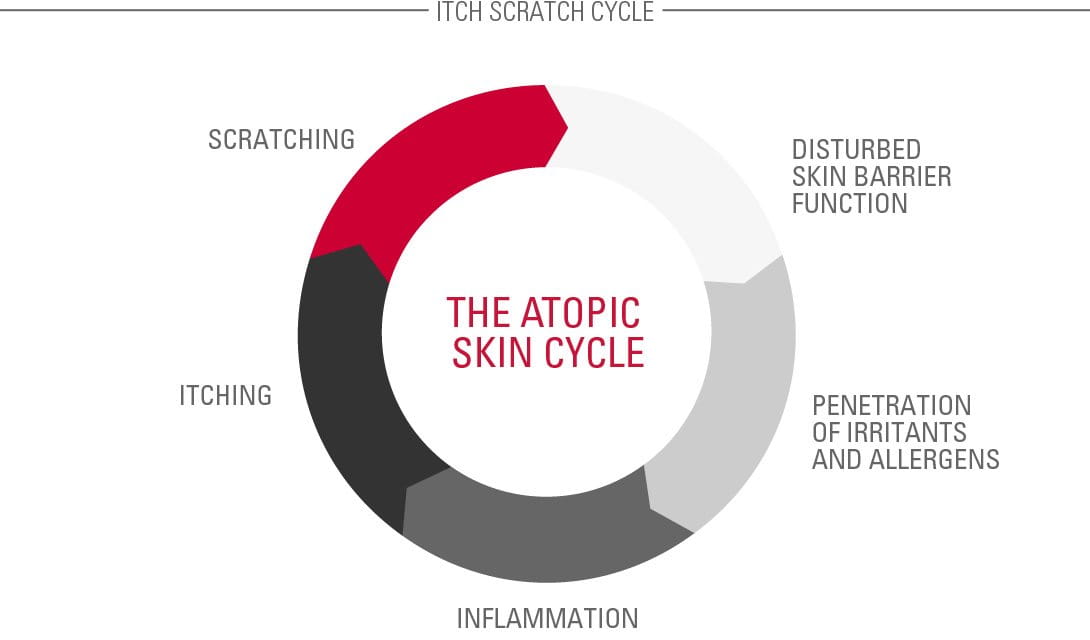
Problems are often caused by the Atopic Skin Cycle. This begins when a child scratches an itch and disturbs their already fragile skin barrier.
This causes a bacteria called Staphylococcus aureus to multiply and infect the skin.
The infection causes inflammation, which causes itching. The cycle starts all over again.
Treatments help to break the Atopic Skin Cycle.
Contributing Factors
Further contributing factors
Certain foods, drinks, textures and textiles are thought to cause or affect atopic skin.
These include:

- Materials like wool and nylon which can be abrasive and cause skin to sweat
- Food allergies, most commonly milk products, nuts and shellfish (speak to a doctor before removing any foods from a child’s diet)
- Allergies to house mites, dust or pollen
- Washing detergents
- Make-up (although sensitive skin brands should be fine)
- Passive cigarette smoke
Some of the side-effects of the disease – such as stress and sleeplessness – can also make symptoms worse.
Read more about factors that influence skin.
Solutions
Managing the symptoms of facial Atopic Dermatitis in children
It can be extremely distressing for parents to see their child suffering but although there’s no cure for Atopic Dermatitis, regular and consistent treatment can help prevent the disease getting worse, calm the skin – relieving pain and itch – reduce emotional stress, prevent infections and stop the skin from thickening.
A treatment plan will probably include a skin care regime as well as some lifestyle changes.
For non-flare phases, daily use of emollients is vital.
Emollients
Emollients, or moisturisers, include lotions, creams, face creams and bath and shower oils, all of which work together to keep skin hydrated, supple and protected from irritants. Their regular use is fundamental to the care of atopic skin and might prolong the non flare-up phases. Children and babies with facial Atopic Dermatitis should apply moisturising face creams at least twice a day.

Key ingredients in the formulas of emollients can include:
- Omega-6-fatty acids from Evening Primrose Oil and Grape Seed Oil. These soothe and nourish the skin while replenishing skin’s natural protective barrier.
- Licochalcone A (an extract of the licorice root). This is a natural anti-inflammatory and antioxidant which reduces redness and soothes inflammation.
Active care
When flare-ups occur emollients need to be used in conjunction with active care treatments such as topical creams and anti-itch sprays. These topical creams usually contain corticosteroids like hydrocortisone.

Hydrocortisone is known to be effective and fast-acting and it alleviates the itching of flare-ups. However, many parents feel uncomfortable about using it on childrens’ skin as prolonged use can have several negative side effects. Also, it loses its effectiveness if used continuously and it can’t be used on large areas of skin.
Eucerin‘s AtoControl Acute Care Cream has skin caring properties that have been clinically proven to significantly improve the skin‘s appearance during flare-up phases. This caring skin solution helps reduce the use of hydrocortisone during flare-ups. Eucerin AtoControl Acute Care Cream is not a pharmaceutical product and is not meant to replace one.
Further advice for parents with children with facial Atopic Dermatitis

- Use warm water for washing, not hot.
- Pat skin almost dry, then apply the emollient straight away.
- Apply emollient at least twice a day.
- Keep fingernails short and smooth so the child cannot scratch and puncture the skin.
- Put cotton gloves on the child at night to prevent face scratching in their sleep.
- Keep room temperatures cool and humidity low.
- It can be a good idea to give a child a doll to scratch as this can reduce their need to scratch their own skin.
Our brand values

We deliver a holistic dermo-cosmetic approach to protect your skin, keep it healthy and radiant.

For over 100 years, we have dedicated ourselves to researching and innovating in the field of skin science. We believe in creating active ingredients and soothing formulas with high tolerability that work to help you live your life better each day.

We work together with leading dermatologist and pharmacist partners around the world to create innovative and effective skincare products they can trust and recommend.




