Atopic Dermatitis is a very common, chronic skin disease that affects adults, children and babies. Skin on the face and body is very dry and irritable. Typically Atopic Dermatitis has two phases, active (also known as ‘flare-ups’ and inactive. It is important for sufferers to protect skin during inactive phases to prolong the periods between active phases.
Signs & Symptoms
What is Atopic Dermatitis?
Atopic Dermatitis (or Atopic Eczema) is a non-contagious chronic disease in which skin on the face and/or body is constantly dry, itchy and irritable. In other words, it is an inflammatory illness – and one that is becoming increasingly prevalent, particularly in the Western world. It affects 10% of the global population (between 10-20% of children and 2-5% of adults are affected) and, over the past 30 years, cases have grown by 200-300%.
Babies and small children are most commonly affected. 90% of patients experienced symptoms before the age of five and 80% before the age of two.
In young children and babies, the most commonly affected area of skin is the face although, as they get older, the rash may spread to the body. Facial Atopic Dermatitis affects all ages and usually appears as dry and scaly patches on the scalp, forehead, round the eyes and behind the ears. Outbreaks are also very common on the cheeks, particularly in babies.
Symptoms differ from person to person, from season to season, even from day to day. Sufferers describe two distinct phases in atopic skin – inactive („interval“) and acute (“flare-ups”).


In an acute flare-up sufferers experience: light to intense itching and skin that is red to deep red, flaky, uneven to swollen, sore and even mildly bleeding.
During a non flare-up phase, symptoms are dry to very dry, slightly flaky, irritable skin (a condition - not a disease - also known as Xerosis) and the affected area may have small, healed cracks.
As well as the problems caused by the skin irritation itself, Atopic Dermatitis can lead to further physical and psychological issues such as lack of sleep, discrimination, stress and a general lack of self-confidence – particularly in the case of facial Atopic Dermatitis. As a result, sufferers often restrict their daily lives by changing what they wear, what they eat, the make-up they choose and the activities they take part in. Relationships can even be affected if the sufferer feels his or her attractiveness is diminished by their symptoms.
You might have Atopic Dermatitis if…
- Your skin is dry and reddened and, unlike dry and very dry skin, it cannot be cured, only managed.
- Your skin is prone to scaling, thickening and cracking. Skin is intensely itchy and has a tendency to reddening and inflammation. This is not only caused by moisture deficiency but also a disruption of fatty acid metabolism which leads to a breakdown of the skin barrier function.
- Your dry skin experiences flare-ups.
Attention
If you are unsure about your symptoms seek the advice of a doctor or dermatologist.
Causes & Triggers
Potential causes and triggers of Atopic Dermatitis
There is no proven single cause for Atopic Dermatitis. Nor, sadly, is there a cure. However, avoidance of triggers and daily proactive intensive care can prolong the healthy phases of atopic skin while acute treatment offers quick relief and recovery from flare-up symptoms.
There are a number of genetic and environmental theories as to why some people develop Atopic Dermatitis and others don‘t. These include:


- Genetic links. Atopic Dermatitis is the most common form of eczema and is closely linked with asthma and hay fever.
If both parents have Atopic Dermatitis, their child has an 60-80% chance of inheriting its parents’ disease.
- Climate/Pollution. Living in a developed country, a city (especially one with higher levels of pollution) or a cold climate seems to increase risk. For example Jamaican children in London are twice as likely to develop Atopic Dermatitis as those who live in Jamaica.
- Gender. Females are slightly more prone to Atopic Dermatitis than males.
- Mother’s age when the child is born. The older the mother, the higher the chances of a child developing Atopic Dermatitis.
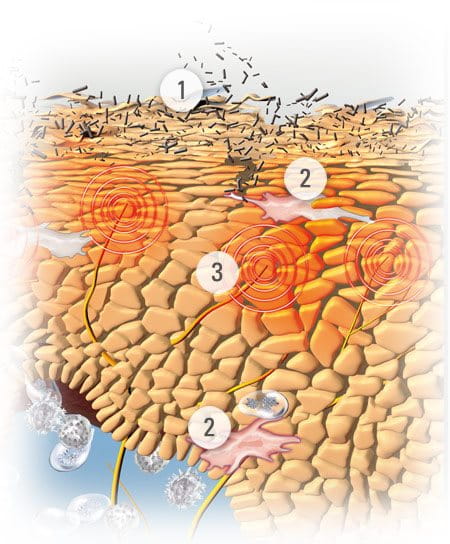
There are four pathogenetic factors of Atopic Dermatitis:
1. Hereditary filaggrin deficiency; a deficiency of natural moisturising factors (NMF) such as amino acids.
2. Disturbed epidermal lipid metabilism (ceramides, cholesterol and free fatty acids) and impaired barrier lipid formation.
These lead to dry skin with a disturbed barrier function. This then makes it easy for infectious agents to penetrate:
3. Bacteria growth (Staphylococcus aureus) and the secretion of super-antigens.
4. Environmental influences such as irritants, allergens, pollution.
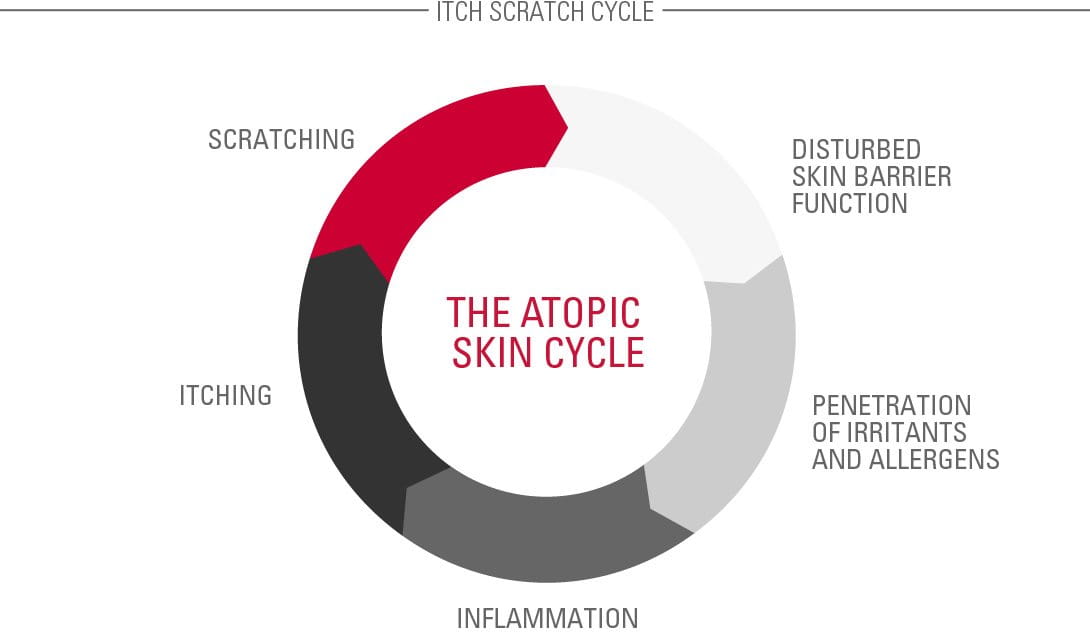
Dry, irritated skin results in inflammation and itchiness. Constant itchiness can lead to constant scratching. This disrupts the skin barrier, which results in a humid growth environment for bacteria. This, in turn, causes irritation and subsequent itching and inflammations. And so the Atopic Cycle continues (see illustration).
Contributing Factors
Further contributing factors
There are a number of other influences that can aggravate existing symptoms, although these vary from person to person. These include:

- certain foods and drinks (notably dairy products, nuts, shellfish and alcohol)
- allergens (house mites, pollen and/or dust)
- formaldehyde
- washing detergents
- stress
- sleeplessness
- sweat
- cigarette smoke
Read more about factors that influence skin.
Solutions
Controlling the symptoms of Atopic Dermatitis
Although there is no ‘cure’ for Atopic Dermatitis symptoms can be managed through consistent and regular care.
Emollients


Emollients (also called moisturisers) are key to this skincare and these should be used every day, regardless of whether the sufferer is in an active or inactive phase. These include lotions, face creams, ointments and bath/shower additives which oil the skin and help keep it supple, moist and protected from irritants. This also helps to prevent itch and may reduce the frequency of flare-ups.
The role of emollients is to prevent Atopic Dermatitis from flaring up. This is known as basic care.
With facial Atopic Dermatitis it is particularly important that moisturisers form part of the daily face care routine.
Key ingredients in emollients can include:
- Omega-6-fatty acids from Evening Primrose Oil and Grape Seed Oil. These soothe and nourish diseased skin while replenishing skin’s natural protective barrier.
- Licochalcone A (an extract of the licorice root). This is a natural anti-inflammatory and antioxidant which reduces redness and soothes inflammation.
Dermatological treatments
Medicinal treatments, such as topical ointments (usually containing hydrocortisone), tackle the symptoms of flare-ups and help to reduce any inflammations and itching.

Corticosteroids are very effective and fast-acting and alleviate itching in cases of severe flare-up. However, it is not a long-term sustainable option as prolonged can have negative side effects. Also, it can’t be applied on large skin areas and it loses efficacy with continuous use.
Daily personal care for facial Atopic Dermatitis

- Cool temperatures, particularly at night, are helpful because sweating causes irritation and itch.
- Basic care products are best kept in the fridge as the application of cooled creams and lotions offers additional itch relief.
- Make-up can be worn but it is best to use products for sensitive skin.
- A diary can help with monitoring whether certain foods or drinks influence symptoms
- Holiday destinations in climate-therapy locations, such as the North Sea, Atlantic, Dead Sea, Mediterranean Sea or high mountain areas may be helpful.
- Relaxation exercises such and yoga and meditation can help reduce stress – one of the factors that can affect facial Atopic Dermatitis.
- When itching occurs, it is better to pat the skin rather than scratch it. Patting soothes skin but doesn’t damage it. After showering, gently pat skin almost dry then immediately apply cream/lotion.
- Keep children’s nails short and smooth to avoid scratch infections.
- Avoid mechanical irritations such as harsh sponges.
Attention
If you are unsure which management route to take please seek the advice of a doctor or dermatologist.
Our brand values

We deliver a holistic dermo-cosmetic approach to protect your skin, keep it healthy and radiant.

For over 100 years, we have dedicated ourselves to researching and innovating in the field of skin science. We believe in creating active ingredients and soothing formulas with high tolerability that work to help you live your life better each day.

We work together with leading dermatologist and pharmacist partners around the world to create innovative and effective skincare products they can trust and recommend.



