Atopic Dermatitis is a skin disease that affects between 2-5% of adults and as many as 10-20% of children globally. It is a chronic, long-term condition characterised by dry, flaky, irritable skin and occasional flare-ups with more distressing symptoms. While there’s no known cure, regular and consistent skin care can protect skin.
Signs & Symptoms
What is Atopic Dermatitis?
Atopic Dermatitis – also known as Atopic Eczema – is a chronic skin disease that affects the skin on the face and body of babies, children and adults.

Incidences are on the increase, particularly in the Western world, with a two- to three-fold increase in reported cases than there were 30 years ago. There is no conclusive cause known for Atopic Dermatitis but there is evidence of links with both asthma and hay fever.
The disease mainly affects children – 10-20% of children globally are affected – while 2-5% of adults have the condition.
In adults the rash tends to affect the neck and décolleté, the inside of elbows, back of knees, hands and feet, as well as the face and scalp. Symptoms and affected areas are slightly different when it comes to children and babies.
People with Atopic Dermatitis often experience additional problems – such as lack of sleep, stress, discrimination and a lack of self-confidence. As well as maintaining a good skin care routine, there are certain lifestyle changes that can alleviate the symptoms – such as wearing cotton clothing, keeping temperatures low to avoid sweating and avoiding trigger foods.
Attention
If you are unsure about your symptoms seek the advice of a dermatologist.
Causes & Triggers
Potential causes and triggers of Atopic Dermatitis
Dermatologists have yet to discover a definitive cause for Atopic Dermatitis, nor a cure. However, there is evidence of a number of factors that make some people more at risk than others. These include:


- Genetics. There is a proven link between Atopic Dermatitis, asthma and hay fever. If one or both parents suffer from one of these conditions, there is a chance that their child will develop Atopic Dermatitis. The risk increases proportionally so if both parents have all three conditions, the chance of the child inheriting the disease increases.
- Climate/location. Cold climates put people more at risk of Atopic Dermatitis, as do polluted cities. There is evidence that Jamaican children brought up in London are twice as likely to develop Atopic Dermatitis as their peers in Jamaica.
- Gender. Females are slightly more prone to Atopic Dermatitis than males.
- Mother’s age. Children born to mothers late into their childbearing years are at a higher risk than those born to younger mothers.
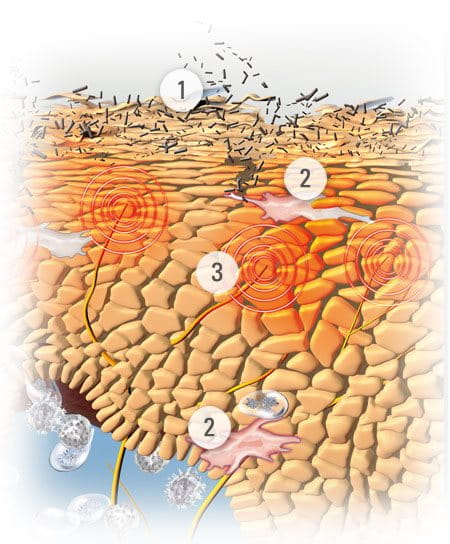
Atopic skin lacks natural moisturising factors (NMF´s), such as amino acids, and has impaired barrier lipid formation. This makes the skin barrier weak and underlying layers prone to infection caused by nails scratching through the skin surface.
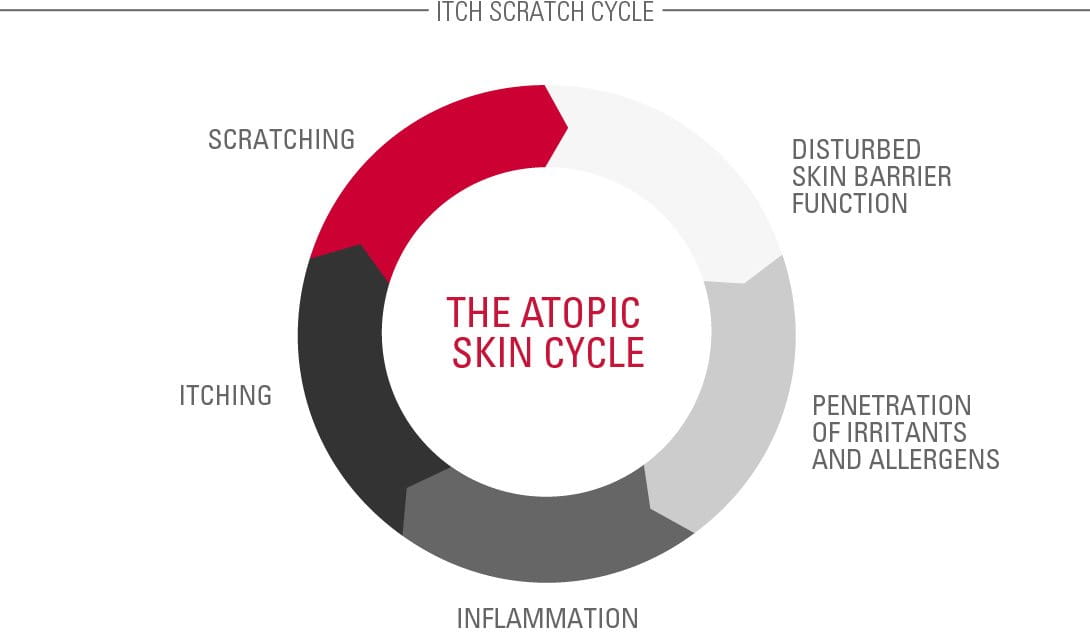
The symptoms of Atopic Dermatitis are also the triggers. Because skin is dry and itchy, sufferers scratch. By scratching, they disturb the skin barrier function. This leaves underlying layers exposed and vulnerable to infection from the environment. The bacteria causes irritation and so the itching continues. This is known as the Atopic Skin Cycle.
contributing factors
Further contributing factors
Other influences that can aggravate existing symptoms, although different people have different triggers, include:

- food allergies – eg. milk, cheese, nuts, shellfish
- alcohol allergies
- allergies to house mites, pollen and/or dust
- abrasive or non-breathable fabrics – eg. wool and nylon
- nickel – a common metal found in jewelry and watches
- formaldehyde
- certain washing detergents – often labeled ‘biological’
- stress
- sleep deprivation
- sweat
- cigarette smoke
Read more about factors that influence skin.
Solutions
Controlling the symptoms of Atopic Dermatitis on the body
There is no known cure for Atopic Dermatitis but there are a number of ways that sufferers can help to care for their atopic skin and perhaps even prolong the periods between flare-ups.
The most important is keeping skin constantly moisturised with emollients.
Emollients
Emollients (also known as moisturisers) must be applied daily, regardless of symptoms. These lotions, face creams, shower oils and bath additives keep skin supple and moist, and therefore less susceptible to itching and damage. Regular use of emollients helps to reduce itching.
Active ingredients often found in formulas of emollients include:
- Omega-6-fatty acids from Evening Primrose Oil and Grape Seed Oil. These soothe and nourish the skin while replenishing skin’s natural protective barrier.
- Licochalcone A (an extract of the licorice root). This is a natural anti-inflammatory and antioxidant which reduces redness and soothes inflammation.
Dermatological treatments
Flare-ups require more intensive care with acute creams being added to the daily moisturising routine. These topical creams often contain hydrocortisone.


Corticosteroids (such as hydrocortisone) are known to be effective and fast-acting in alleviating itching and reducing inflammation. However, it does have some drawbacks. For example, prolonged use can thin skin.
For that reason it’s not sustainable in the long term, nor is it ideal for use on babies and children.
Eucerin‘s AtoControl Acute Care Cream has skin caring properties that have been clinically proven to significantly improve the skin‘s appearance during flare-up phases. This caring skin solution helps reduce the use of hydrocortisone during flare-ups. AtoControl Acute Care Cream is not a pharmaceutical product and is not meant to replace one.
Daily personal care for Atopic Dermatitis on the body
Although triggers vary from person to person, there are quite a few lifestyle changes that sufferers have found to be effective:


- Keeping room temperatures and humidity low to avoid sweating.
- Wearing clothes that are soft next to the skin. Cotton is comfortable and can be layered in the winter. Scratchy textures, such as wool, and non-breathable fabrics like nylon are best avoided.
- Keeping skin care products in the fridge as cool creams help alleviate itchiness.
- Writing a diary, noting any triggers that cause flare-ups.
- Taking holidays in cool to moderate climates – not too hot or too cold.
- Washing new clothes before wearing them to remove irritating dyes and fabric finishers.
- Wearing cotton gloves at night to prevent scratching during sleep.
- Wet wrap’ therapy can help reduce itch and lessen the desire to scratch (speak to your dermatologist for more information).
- Taking showers rather than baths, but never too hot (<32°) and not too often or too long.
- Limiting bath times to no longer than 5-10 minutes.
- Always using bath oils (or shower oils) as these have a lipid refreshing, caring effect.
- Avoiding any harsh sponges or massage brushes in the bath or shower.
- Doing mediation and yoga to relieve stress.
Attention
If you are unsure which management route to take please seek the advice of a dermatologist.
Our brand values

We deliver a holistic dermo-cosmetic approach to protect your skin, keep it healthy and radiant.

For over 100 years, we have dedicated ourselves to researching and innovating in the field of skin science. We believe in creating active ingredients and soothing formulas with high tolerability that work to help you live your life better each day.

We work together with leading dermatologist and pharmacist partners around the world to create innovative and effective skincare products they can trust and recommend.




