Atopic Dermatitis is a very common skin disease that affects the face and body, where skin is constantly dry and irritable. Sufferers report two phases. An inactive phase (which they also call “interval“) where facial skin is dry and irritable, but symptoms can be managed, and an active phase, also known as the “flare-up” phase, where skin becomes inflamed and itchy. During a flare-up, a more active skin routine, using cosmetic skin care and/or pharmaceutical treatments, may be required.
Signs & Symptoms
What is Atopic Dermatitis?
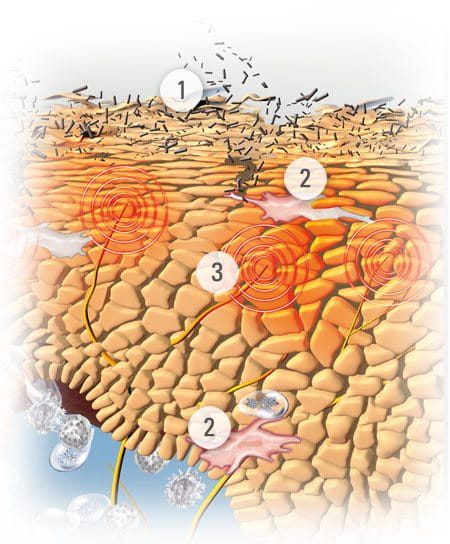
Atopic Dermatitis (also known as Atopic Eczema) is a chronic skin disease that affects babies, children and adults – on the body as well as the face. It is characterised by dry, irritated and itchy skin which becomes thickened and can crack and sometimes bleed. There is no single known cause but sufferers do have a moisture deficiency and disruption of fatty acid metabolisms which lead to a breakdown of the skin barrier function.

Around 10% of the global population (between 10-20% of children and 2-5% of adults are affected) and cases are on the increase. In fact, over the past 30 years patient numbers have grown by 200-300%.
Atopic Dermatitis is most common in babies and children. 90% of patients experienced symptoms before they were five and 80% by the time they were two. Evidence suggests that there are slightly more female than male sufferers and it is predominantly a disease of the Western world.
Atopic skin goes through two phases: non-active (or “normal”) and active (or “flare-up”).
During a non-active phase facial skin may be dry to very dry, slightly flaky, pink to red and affected areas – most commonly the cheeks, scalp, forehead, round the eyes and behind the ears - may have small healed cracks.
The more distressing phase, both physically and psychologically, is the flare-up phase when sufferers experience light to intense itching and facial skin that is red to deep red, uneven to swollen, sore, flaky and even mildly bleeding.
Attention
If you are unsure about your symptoms seek the advice of a doctor or dermatologist.
Causes & Triggers
Potential causes and triggers of Atopic Dermatitis
As yet, no single cause has been identified although a number of factors are thought to contribute to Atopic Dermatitis.


For example:
- There are proven links between Atopic Dermatitis, hay fever and asthma, and evidence shows that if one or both parents suffer from any or all of these conditions, their child is more likely to develop Atopic Dermatitis. In fact if both parents have atopic skin, there is a 60-80% chance their child will too. Children inherit filaggrin deficiency from affected parents which leaves them lacking natural moisturisation.
- Geographical location can play a major part in the development of the disease. Its prevalence is vastly skewed to the Western world and cases are significantly higher in cities than in the countryside. Cold climates also seem to increase risk. For example, Jamaican children are twice as likely to develop Atopic Dermatitis growing up in London (where pollution is high and temperatures relatively low) than those living in Jamaica.
- There is some evidence that the age of a mother when she gives birth has a direct relationship to the child’s risk of having atopic skin – the older the mother, the higher the chances.
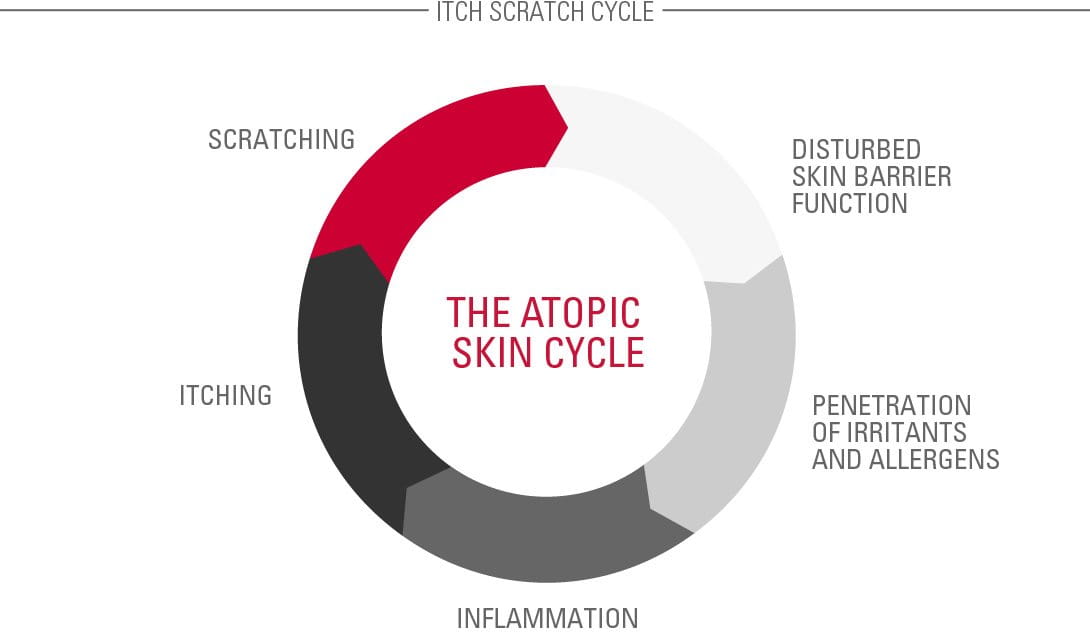
These pathogenetic factors lead to dry skin with a disturbed barrier function.
When sufferers scratch, they damage the skin barrier leaving underlying layers prone to bacteria infection and environmental influences such as irritants, allergens and pollution.
contributing factors
FURTHER CONTRIBUTING FACTORS


There are a number of other textures or chemicals that can contribute to, or aggravate, existing symptoms, such as:
- clothing or materials – particularly wool and nylon
- certain foods – dairy, nuts, shellfish etc.
- alcoholic drinks
- allergies to house mites, dust or pollen
- washing detergents
- formaldehyde
- cigarette smoke
As well as emotional triggers that can affect the sufferer’s symptoms including:
- stress
- sleeplessness
- sweat
Read more about factors that influence skin.
Solutions
Managing the symptoms of Atopic Dermatitis in a flare-up
Although there is no ‘cure’ for Atopic Dermatitis, inactive and active flare-up symptoms can be alleviated with cosmetic skin care and pharmaceutical products.
Emollients
During inactive phases, emollients (or moisturisers) must be used regularly and consistently every day. These creams, lotions and oils contain high concentrates of oil so help keep skin supple, moist and protected from irritants. Because skin is moisturised it is less itchy and the skin barrier is less likely to be damaged by scratching.
Ingredients often found in emollients include:
- Omega-6-fatty acids from Evening Primrose Oil and Grape Seed Oil. These soothe and nourish diseased skin while replenishing skin’s natural protective barrier.
- Licochalcone A (an extract of the licorice root). This is a natural anti-inflammatory and antioxidant which reduces redness and soothes inflammation.
Active care
During flare-ups more active care is required to help reduce any inflammations and itching. Pharmaceutical products tend to use corticosteroids as they are very effective and fast-acting and alleviate itching in case of severe flare-up. However, hydrocortisone is not a long-term sustainable option – particularly for babies and children - as prolonged use may thin skin. Also, it can’t be applied on large skin areas and its effectiveness is diminished with continuous use.


Eucerin’s AtoControl Acute Care Cream‘s skin caring properties significantly improve the skin‘s appearance during flare-up phases and helps reduce the use of hydrocortisone during flare-ups. AtoControl Acute Care Cream is not a pharmaceutical product and is not meant to replace one.
Daily personal care for facial Atopic Dermatitis
Sufferers can also make changes to their lifestyles to help alleviate their discomfort.

For example:
- Keeping temperatures cool - particularly at night. Sweating causes irritation and itch.
- Keeping creams and ointments in the fridge as cooled emollients offer additional itch relief.
- Maintaining a diary of environmental and nutritional behaviour to identify any trigger symptoms.
- Taking holidays in climatically sensitive locations such as the North Sea, Atlantic, Dead Sea, Mediterranean Sea or high mountain areas.
- Doing yoga or meditation to help reduce stress.
- Patting rather than scratching skin. While both soothe skin, patting doesn’t damage the skin barrier.
- Keeping children’s nails short and smooth to minimise damage caused by scratching.
- Wearing cotton gloves at night to prevent scratching the face during sleep.
- Taking showers rather than baths, keeping the temperature below 32° and not showering too frequently.
- Patting skin almost dry, then applying cream or lotion directly after.
- Avoiding irritants such as harsh sponges.
Attention
If you are unsure which management route to take please seek the advice of a doctor or dermatologist.
Our brand values

We deliver a holistic dermo-cosmetic approach to protect your skin, keep it healthy and radiant.

For over 100 years, we have dedicated ourselves to researching and innovating in the field of skin science. We believe in creating active ingredients and soothing formulas with high tolerability that work to help you live your life better each day.

We work together with leading dermatologist and pharmacist partners around the world to create innovative and effective skincare products they can trust and recommend.



